The immune system – the body’s protective shield
The immune system protects us from threats encountered in our busy environment by fighting microorganisms that have invaded the body, such as bacteria, fungi and viruses, or by preventing them from entering the body in the first place. Foreign substances and defective or dead cells from within the body can also trigger the immune defenses.
In order to carry out its function of maintaining the body’s integrity, the immune system must be able to differentiate between the body’s own cells and foreign cells. If it is not able to, then either the immune defenses are weakened or autoimmune diseases can arise in which immune cells attack the body’s own tissues. In order for the defense system to function properly, it is necessary for the numerous elements of the immune system to be finely coordinated. Ideally, the immune system should be in equilibrium. In other words, it responds forcefully to pathogens.
Here you will find information about these topics

How the immune system is structured
Our complex defense system involves various organs, cells and specialized proteins located throughout the body. It comprises two parts: the innate or non-specific immune system and the adaptive or specific immune system. Both systems include specialized immune cells in the form of white blood cells, or leucocytes (= cellular component), and blood proteins (= soluble component) such as antigens. They are closely interconnected.
TWO-PART IMMUNE SYSTEM
The innate immune system
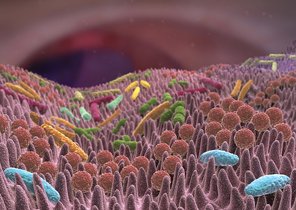
The bacteria in the skin and intestinal flora also play an essential part in the immune defenses of the human body.
It is present from birth and in many cases actually prevents pathogens from invading the body and facilitates a rapid immune response. Although it cannot adapt to new pathogens, its various responses provide an effective defense in many situations.
Impermeable interfaces provide an effective barrier
Mechanical barriers with different physiological defense mechanisms are the first line of defense. Our skin and mucous membranes – the respiratory tract, the eyes, the gut or the reproductive organs – form interfaces with the external environment. As they represent a potential portal of entry for pathogens, this is where the initial immune responses occur. That being said, intact cell organization already ensures good mechanical protection. This requires healthy cells and tight junctions between the cells.
Also, in play are biochemical substances such as sweat, saliva and mucus, which additionally contain antimicrobial proteins. Gastric acid also plays its part; thanks to its very low acidic pH it is able to kill numerous potential pathogens. The physical removal of pathogens or unwanted substances is facilitated either by cilia, for example in the respiratory tract, fluids such as tears, nasal secretions and urine, or bowel movements. The bacteria that colonize the human body also play an essential part in the immune defense – both the skin flora and especially the representatives of the intestinal flora (more on this below).
Multifaceted cellular defense
If pathogens – bacteria, parasites, fungi and viruses – overcome these barriers, white blood cells – leucocytes – come into play. These blood cells originate in the bone marrow and do not carry haemoglobin. Instead, they can
differentiate between the surface structures of the body’s own cells and foreign cells,
release various signal substances, thereby triggering inflammation,
produce antibacterial proteins such as lysozyme or
ingest and digest (phagocytosis) pathogens such as dead, defective or altered cells, e.g. virus-infected cells and tumor cells, from within the body – they are then called phagocytes.
White blood cells circulate in the blood, but they are capable of active movement and can therefore also migrate into tissue. Leucocytes include dendritic cells, granulocytes (basophils, eosinophils, neutrophils), macrophages and their precursor cells, the monocytes, but also mast cells and natural killer cells. Killer cells bring about the cell death of altered cells from within the body, such as virus-infected cells and tumor cells.
Another element of the non-specific immune system is the complement system, which consists of specific proteins that are activated via a cascade. Their main role is to tag pathogens so that it is easier for immune cells to identify and attack them. In addition, these proteins can trigger inflammation and destroy bacterial envelopes.
Inflammation can also be beneficial
Inflammation is an immune response to harmful stimuli induced by signal substances (e.g. cytokines). It should result in more rapid healing, by attracting immune cells that remove or destroy foreign substances and pathogens.
However, the body’s own tissues can be damaged in the process, which is why severe and especially also recurrent inflammation is problematic. If inflammation is directed against harmless environmental stimuli such as pollen, experts call this an allergy, which is generally caused by the adaptive immune system. When the inflammatory response targets the body’s own structures and cells, this is known as autoimmune disease.
The adaptive immune system
While the innate immune system responds non-specifically to a wide range of stimuli, the adaptive immune system acts against specific antigens.
The adaptive immune system develops throughout our life and is fully formed from puberty. The key fact: it can adapt to new or altered pathogens. Protein, lipid and carbohydrate compounds or complex molecules on the cell surface act as antigens. White blood cells in the form of B and T lymphocytes (B and T cells) carry receptors on their surface that can only bind to specific antigens, like a lock-and-key system.
Various cells, such as dendritic cells, present antigens from pathogens on their cell surface following phagocytosis of the pathogens. B cells with corresponding receptors respond to the relevant antigens by transforming into plasma cells and producing corresponding antibodies. The antibodies bind to the respective antigens, thereby
blocking the antigens and inhibiting their harmful effect;
tagging pathogens for phagocytes;
activating the complement system, whose components destroy the tagged cell;
tagging altered endogenous cells for natural killer cells.
T cells recognize the body’s own cell surface structures and respond to altered or foreign structures on body cells by differentiating into so-called effector cells: as killer T cells they destroy altered cells, as T helper cells they attract other immune cells or activate B lymphocytes, and as regulatory T cells they protect intact body cells. Regulatory T cells thereby direct the immune response, aid immune tolerance and prevent autoimmune diseases.
As it can take around four to seven days until the adaptive immune system is able to fight foreign pathogens that it has encountered for the first time, the innate immune defense system is required initially. However, both B and T lymphocytes form long-lived memory cells which produce antibodies and effector T cells much more rapidly when they come into contact with the same pathogen again. In the best case, they ensure lifelong immunity to the relevant pathogen. Vaccines also make use of the principle of memory formation.
Bacteria ensure a well-functioning defense system
Microorganisms, more specifically bacteria, are an essential element of an effective defense system. They colonize our skin and mucous membranes in large numbers. The resident bacteria in the microflora oust harmful bacteria, boost the skin and mucous membrane barriers and also interact with our immune system by stimulating the formation of antimicrobial defensive substances, for example. In general, the immune system only develops properly when it comes into contact with bacteria – in particular with the physiological representatives of the intestinal flora. This has been demonstrated by studies of pathogen-free animals raised in sterile conditions in a laboratory, which only have a partially developed immune system.
Our skin is covered by a protective acid mantle that produces sweat and sebum. This water-lipid film protects the skin from drying out and also from harmful microorganisms. The mildly acidic pH (around 5.5) of the acid mantle favors the growth of natural bacterial flora and enhances the action of the fatty acids and enzymes it contains, which target fungi and pathogens.
Our digestive tract provides an especially large surface area, in particular the gut, which when unfolded has a significantly larger surface area than the skin, which covers around two square meters. With every bite of food, we take, we also ingest foreign substances and potentially harmful microorganisms. Due to the close contact between allergens such as bacteria and the body’s own structures, the gut contains around 70 to 80% of all immune cells in the body. They lie directly under the single-layer intestinal mucosa and also between the intestinal epithelial cells. The gut therefore represents the headquarters of our immune system, and its immune defenses have an impact on all other areas of mucous membrane in the body.
